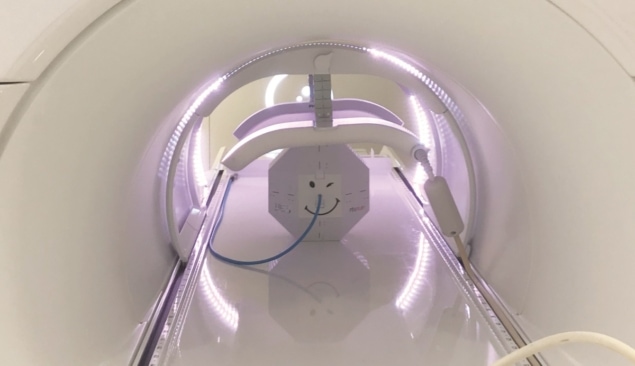
PTW’s modular RUBY phantom is being optimized to support daily and end-to-end quality assurance (QA) for the Elekta Unity MR-Linac treatment system
The Elekta Unity MR-guided radiotherapy (MR/RT) system is rewriting the rulebook in radiation oncology, opening up new possibilities for the visualization of the tumour target, as well as its surrounding anatomy, with exceptional soft-tissue contrast both prior to and during treatment. While it’s still early days for MR/RT deployment, the anticipated patient outcomes – when realized at scale – already look compelling. Consider the fundamental biology: tumour shape and position relative to healthy tissue evolve over the course of a radiotherapy treatment programme – and can even change during an individual treatment session. The ability of MR/RT to detect those changes and adapt therapy accordingly – in effect, helping clinicians to “see what they treat” in real-time – means that radiation oncology teams are now able to improve the precision of radiation delivery, more effectively treating the tumour while sparing healthy tissue and minimizing damage to adjacent organs at risk and other critical structures.
If the upward trajectory for MR/RT is clear, the operational reality of adding a 1.5 T MRI scanner into the treatment mix is, unsurprisingly, one of significantly increased system complexity versus more established radiotherapy modalities – not least in terms of defining a rigorous, standardized and streamlined approach to MR/RT quality assurance (QA). For starters, QA products not only need to be compatible with use in a magnetic field – i.e. classified as MR-conditional – they need to be MR-visible as well. Equally important is workflow efficiency: MR/RT QA needs to ensure simple and quick verification of the treatment procedure to confirm that radiation is being delivered to the patient as intended, while at the same time maximizing patient throughput.
The QA challenge
Among a posse of specialist radiotherapy QA vendors addressing this challenge is PTW of Freiburg, Germany, which has developed a portfolio of high-precision dosimetry solutions for MR/RT early-adopters, with products to enable acceptance testing, beam data commissioning, as well as machine- and patient-specific QA. The latest addition to PTW’s MR/RT product line is the RUBY QA phantom, which comes with a variety of exchangeable, application-specific inserts to enable medical physicists to verify the entire radiotherapy equipment chain – from imaging and treatment planning through targeting, dosimetry and delivery.

“One of the main advantages of RUBY is its modularity – comprising a base phantom with a series of inserts for different QA tasks,” explains Daniela Poppinga, a research scientist and product manager at PTW. The daily couch-check, for example, uses the linac QA insert plus base phantom, while there’s a system QA insert for the end-to-end QA. The latter includes MR-visible elements, CT-visible inhomogeneities, as well as the option to insert a detector for dose measurements. “For the end-to-end test,” adds Poppinga, “the user can see the system QA insert in their MR images. With this insert it’s possible to test the whole MR-Linac workflow chain – basically every step the patient goes through.”
It’s worth noting that RUBY was originally developed to support other advanced treatment modalities – including intensity-modulated radiation therapy (IMRT), volumetric modulated-arc therapy (VMAT) and hypofractionated procedures such as stereotactic body radiotherapy (SBRT). Subsequently, the phantom and inserts have been optimized for MR/RT QA testing – a product development initiative that’s been shaped with first-hand inputs from clinical scientists in the department of radiation oncology at University Hospital Tübingen, Germany. “We’re impressed with the functionality of the RUBY phantom,” says Marcel Nachbar, a medical physicist with QA responsibility for the Tübingen clinic’s Elekta Unity system. “One of the neat aspects of RUBY is its multipurpose functionality, such that inserts for the Elekta Unity MR-Linac can be deployed on our conventional linacs as well.”
The QA opportunity
In September 2018, University Hospital Tübingen was among the first clinical sites to start treating patients with the Elekta Unity MR/RT machine – since when Nachbar and his colleagues have delivered well over 3000 treatment fractions with Unity. “Daily QA is pretty straightforward and comprises mostly checks of the MR system [signal-to-noise and scaling factors] and workflow checks,” explains Nachbar. There are other weekly, biweekly and monthly checks, though, that go above and beyond what’s needed for conventional RT linacs. “We have MR QA, linac QA and hybrid/end-to-end QA to evaluate the effective interworking between the MR and linac systems,” he adds.

Operationally, the PTW–Tübingen collaboration looks like a win-win: the Tübingen team gets to evaluate the RUBY phantom for future deployment in its Unity workflow; meanwhile PTW gains insights from the clinical “sharp-end” to inform ongoing requirements-gathering for RUBY innovations tailored to MR/RT daily and end-to-end QA. With this in mind, Poppinga and Nachbar formed part of a joint project team that recently evaluated the use of RUBY (plus patient QA insert) for treatment plan verification in combination with the Unity imaging system MVIC. “We were able to verify the treatment for one complex small-volume case,” explains Nachbar. “We used the PTW detector insert combined with a micro ionization chamber [PinPoint 3D] to get an excellent representation of this small target volume, with the differences between measurements and treatment planning system all within 2%.”
Meanwhile, a second study evaluated the use of RUBY (plus system QA insert) as an end-to-end phantom for Elekta Unity – specifically to address the complexities associated with adaptive MR/RT. In this case, the PTW–Tübingen scientists showed that both of the possible Unity workflows could be fully tested with RUBY – i.e. “adapt-to-position” (in which the dose distribution is repositioned on a daily basis to track changes in tumour position) and “adapt-to-shape” (with daily recontouring and reoptimization to take account of rotation or deformation of the tumour target or nearby organs at risk).
“On end-to-end testing, the RUBY phantom really did simplify our QA workflow,” Nachbar concludes. “As such, it’s clear that RUBY can already be implemented as is for point-dose MR/RT treatment plan verification and end-to-end QA.” Looking ahead, though, Nachbar also sees plenty of scope for the RUBY phantom to streamline and consolidate other MR/RT QA checks into a single platform – for example, monitoring the difference between the MR and MVIC isocentre, the stability of which needs to be tested on a weekly or biweekly basis.
