 Frontiers in Oncology. The patient, a woman with advanced non-small cell lung cancer and multiple metastases, did not experience any side effects from the high radiation dose she received. The dramatic effectiveness of this combined treatment is spearheading the development of future clinical studies.
Frontiers in Oncology. The patient, a woman with advanced non-small cell lung cancer and multiple metastases, did not experience any side effects from the high radiation dose she received. The dramatic effectiveness of this combined treatment is spearheading the development of future clinical studies.
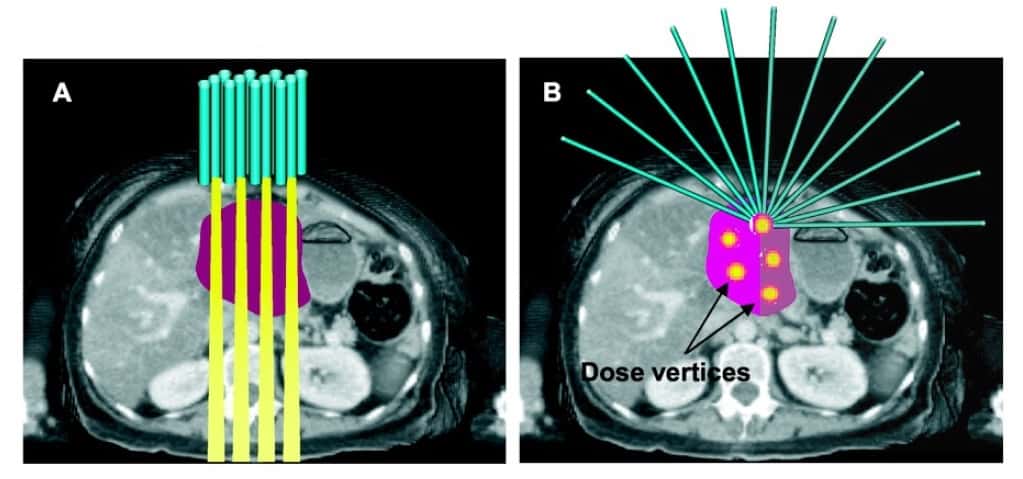
Bulky tumours are challenging to treat using radiotherapy due to large tumour sizes and limitations of normal tissue toxicity. Spatially fractionated techniques such as high-dose 2D grid radiotherapy and LRT – a 3D lattice-like reconfiguration of grid therapy – have been employed to safely treat bulky tumours. LRT uses multiple high-dose regions (vertices), distributed within the tumour volume according to its size and shape and the proximity of critical structures, with valleys of much lower dose in between.
The technique’s principal developer, Xiaodong Wu from Executive Medical Physics Associates in Miami, FL, explains that when 3D LRT is delivered using intensity-modulated radiation therapy, volumetric modulated arc therapy or ion beams, highly customized peak-to-valley dose distributions can be generated within the tumour volume, while sparing skin and normal tissue.
LRT is currently used for palliative tumour debulking or boost treatments and to safely deliver high radiation doses to partial volumes of large tumours. It can be administered alone or in combination with conventionally fractionated radiotherapy.
Led by Benhua Xu, chief of the Department of Radiation Oncology at Fujian Medical University Union Hospital in China, this case study represents the first use of LRT in conjunction with immune checkpoint blockade – a treatment that help the body’s immune system recognize and attack cancerous cells.
The 33-year old patient was diagnosed with advanced invasive adenocarcinoma in the lower lobe of her right lung. Within months following surgery and chemotherapy, she had developed multiple metastases in both lungs, the thyroid, the spine and on the posterior chest wall. While the patient was receiving checkpoint inhibitor therapy, the metastatic mass in the posterior chest wall grew from 2.0 to 63.2 cm3, with maximum dimensions of 5.0 x 5.4 x 5.3 cm.
The team administered a single fraction of LRT (20 Gy prescribed to six high-dose vertices) to this fast-growing mass. The patient continued checkpoint inhibitor therapy, receiving six cycles over the next six months. She also underwent stereotactic body radiotherapy to treat multiple metastases and received drug therapies.
Although all of the patient’s metastatic lesions responded to the various palliative treatments, only the posterior chest wall tumour that received high-dose LRT achieved a complete response. While this tumour had not responded to the initial immune checkpoint blockade (anti-PD1), after high-dose LRT, it shrank by 77.84% within a month and continued to regress until achieving complete local response five months later. There were no toxic side effects in the area of the treatment, and the site remained disease free until the patient died several months later.
The researchers note that with only 6.5% of the large tumour’s volume receiving a dose of 20 Gy and higher, the effective uniform dose was calculated as 1.2 Gy. “Based on the traditionally understood mechanism of radiobiology, the probability of achieving complete local control with such a dose for a tumour of 63 cc would be nearly zero,” they write. “The synergetic effect combining high-dose LRT with anti-PD1 becomes a plausible speculation.”

Carbon ion grid therapy spares healthy tissue
They further hypothesize: “In high-dose LRT, the dose in the vertices are sufficiently high to induce neo-antigen release and initiate the cascade of antigen presenting cell (APC)-based T-cell priming. The dose in between the vertices is low enough to preserve internal tumour circulation/perfusion to potentially facilitate the infiltration of APCs and the primed cytotoxic T-cells. The highly heterogeneous dose configuration could reprogram the immunosuppressive tumour microenvironment to become more immunogenic, and when synergistically treated by checkpoint inhibitors, the primed T cells could attack tumour cells without being exhausted.”
Wu tells Physics World that the researchers are currently preparing systemic clinical studies using this combined treatment for patients with lung cancer, liver cancer, breast cancer and melanoma. He notes that interest in and use of LRT, and spatially fractionated radiotherapy in general, are increasing. Following the early clinical experiences primary made by Innovative Cancer Institute in Miami and Fujian Union Hospital, more institutions, including the Mayo Clinic in Rochester, have begun to offer LRT to their patients.