Wearable sensors that monitor biomarkers in biofluid just under the surface of the skin – wirelessly, painlessly and in real-time – could be of wide medical benefit. Such devices could measure glucose for diabetes management, for example, support the individualization of prescription drug dosing and automatic drug delivery, or even monitor alcohol levels in the body.
Researchers at the University of California San Diego have developed a miniaturized, fully integrated microneedle sensor that continuously monitors glucose, lactate and alcohol levels in interstitial fluid (ISF, the fluid present between cells and tissues) in volunteers. They validated the microneedle-acquired data against parallel lab-based measurements using standard reference methods
Writing in Nature Biomedical Engineering, co-principal investigators Patrick Mercier and Joseph Wang and colleagues describe the initial success of this microneedle technology in accurately monitoring fluctuating levels of single analytes, as well as multiplexed combinations (lactate–glucose and alcohol–glucose), in response to stimuli associated with exercise and food/alcohol consumption.

The sensor technology is based on micron-sized needles that penetrate a few hundred microns into the skin. The small size of such microneedle sensors enables them to be created in a variety of form-factors, such as epidermal patches, and painlessly fixed onto many different locations of the body.
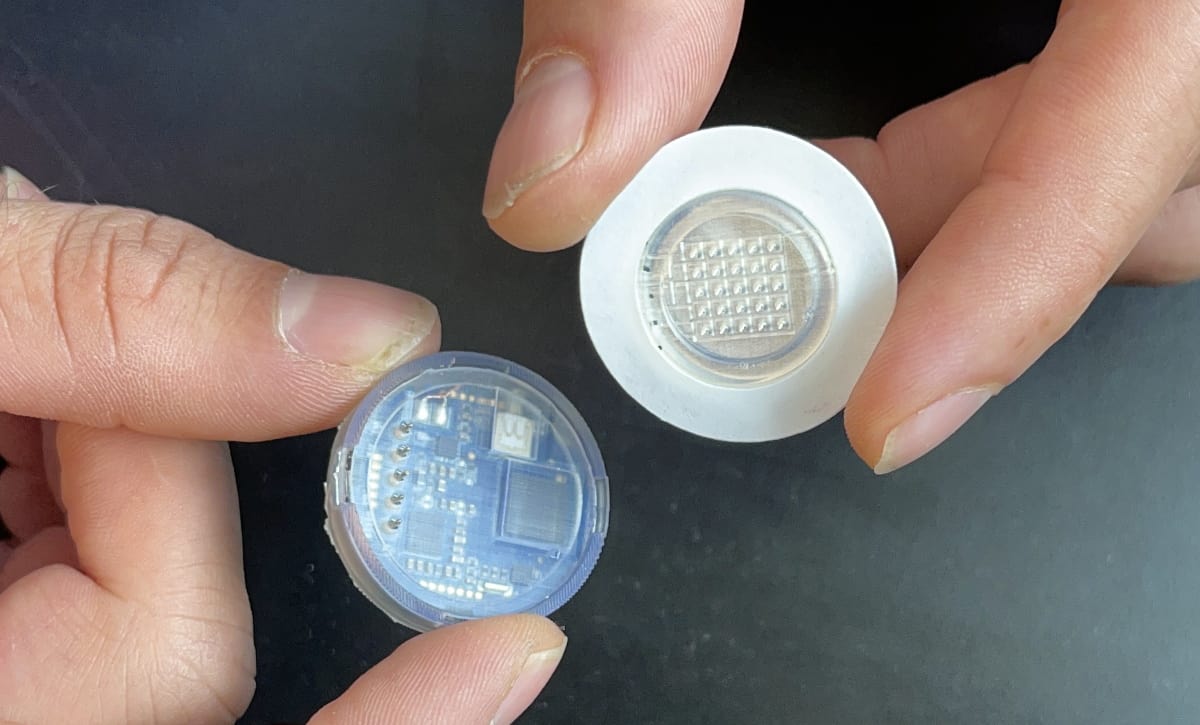
The system, designed for functionality, compactness and low-power operation, consists of a coin-sized layered sensor patch made from two primary components: a disposable sensor (the microneedle array) and reusable electronics (powered by a 30-day rechargeable battery). This design keeps costs low and enables easy replacement of the disposable elements.
The microneedle tips pierce the skin to reach the epidermis, where they continuously and selectively gather molecular-level electrochemical signals from the wearer’s ISF. The signals are carried through the low-noise, reusable sensor’s electronics interface and are wirelessly transmitted to the wearer’s custom smartphone app for visualization and analysis.
Promising results
For the study, five volunteers performed an identical exercise protocol, consumed an identical meal and drank an equal amount of wine to test the sensor’s performance for single-event activities. Multi-event activities included performing low- to high-intensity exercise for 4 min, consuming an entire meal including a dessert, and drinking a glass of wine rapidly and then gradually.
After high-intensity exercise, ISF lactate levels monitored for each participant at 5 min intervals rose rapidly from the resting value, then declined gradually to the original base value. The calibrated ISF lactate levels closely tracked blood lactate measurements taken every 10 min.
Glucose measurements from the microneedle sensor were comparable with blood glucose reference measurements, with data closely reflecting the meal consumed. Of note, each participant had a unique base glucose level in terms of the rates of glucose uptake and glylcolysis. Interestingly, the tests revealed that one of the participants was at increased risk of developing diabetes.
The microneedle sensor produced an instantaneous response to alcohol consumption, which was comparable to data acquired from a breathalyser unit. The researchers report large inter-participant variability and recommend that future research should correlate the ISF data with venous, rather than breath, alcohol levels.
The value of continuous monitoring
Mercier and Wang point out the enormous potential value of this sensor. Lactate data can provide insight into the severity and duration of hyperlactatemia, an elevated blood lactate concentration, in critically ill patients. Lactate levels are also a reliable marker of septic shock, organ failure, trauma or acute inflammatory response syndrome. In an emergency department, continuous lactate sensing can help guide early resuscitation therapies and treatment. Such data may also help athletes reach their maximum body performance and reduce risk of injuries.
Glucose data can be used to monitor plasma glucose levels for diabetic patients, as well as to detect impaired glucose tolerance. Combined monitoring of alcohol and glucose can help diabetic patients from developing delayed hypoglycaemia following alcohol intake.
Monitoring lactate during exercise is also useful for people with diabetes. As physical activity influences the body’s ability to regulate glucose, lactate monitoring can help individualize insulin delivery. Lactate–glucose monitoring, meanwhile, can provide more comprehensive pre-diagnostic information regarding the risk of metabolic syndrome.
Dissolving microneedles could extend access to skin-cancer treatment
Next, the researchers plan to optimize the biosensing chemistry of the sensor system, to mitigate enzyme stability and biofouling issues, and extend wear beyond several hours to several days or even weeks. They also aim to incorporate advanced calibration algorithms into the electronics, integrate other sensors (such as thermal sensors) to compensate for any fluctuations that could affect signal accuracy, and expand the multiplexed sensing capability to additional analytes. The team also intend to conduct clinical trials with large populations to further compare ISF data with centralized laboratory tests.
“By filling the current gaps between research and commercialization, the current work presents a leap forward in the field and can accelerate the emergence of next-generation, patient-centred remote monitoring wearable sensors, thereby offering a pathway to transform digital healthcare as we currently know it,” the researchers conclude.