
Imagine a paediatric intensive care unit (PICU) with no beeping monitors and without tubes, wires and probes lining every inch of each patient’s body – it perhaps seems implausible. While the reality of ICU care today involves wired life-support equipment, a research collaboration centred at Northwestern University envisions a future free of such a daunting environment.
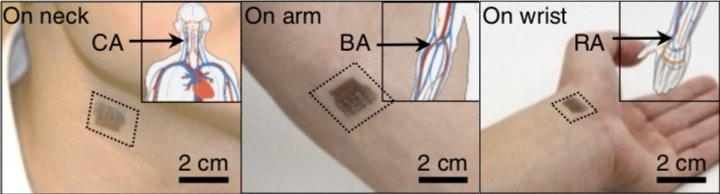
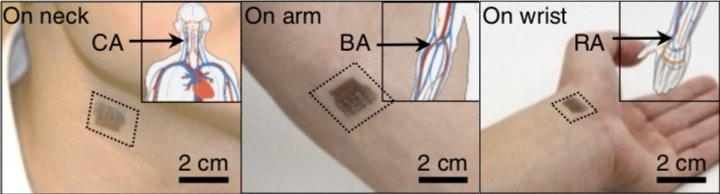
The research team has developed a wireless, skin-interfaced device for non-invasive blood-pressure monitoring, introducing the device in Advanced Healthcare Materials.
Blood pressure monitoring
Tracking the blood pressure of children under intensive care is critical for monitoring their physiological well-being. Extreme low and high blood-pressure events can indicate life-threatening physiological changes such as limited cerebral blood flow.
The “gold standard” method for continuous blood-pressure monitoring of patients in critical care utilizes arterial lines (a-lines). Unfortunately, these catheters are invasive, painful to insert, and associated with risks of infection and limiting blood flow. A-lines are particularly difficult to administer to PICU patients. They are disproportionately sized when compared with children’s small arteries and highly restrictive in nature, often requiring the use of immobilizing accessories such as splints or braces.
The research team’s new device offers a non-invasive alternative to a-lines: a simple skin-interfaced tool for wireless monitoring of blood pressure. To achieve this, the device measures the patient’s heart rate and pulse arrival time (the time for a blood pulse to travel from the heart to the hand or foot), which are calibrated and converted into measurements of systolic and diastolic blood pressure. Doctors require both systolic and diastolic measurements to monitor cardiovascular function and the risk of blood-supply loss in the coronary arteries, a possibly life-threatening condition. The device can be interfaced with smart tablet applications for continuous monitoring and health alerts.
To analyse the proposed model for blood-pressure calibration, clinicians involved with the study collected data from 23 PICU patients. They determined that using a model that combines pulse arrival time and heart rate offered the best means to replicate a-line measurements.
The results indicated that the devices and analysis could meet US Food and Drug Administration specifications for measurements of diastolic blood pressure, while measurements of systolic blood pressure fell just short of the specifications. The researchers note, however, that indwelling a-lines themselves can be subject to over- and underestimation of blood pressure, and suggest that a larger trial would elucidate the validity of their results.
Specialized materials
Over the past decades, medical-device development has moved in the direction of soft devices that replicate the environment in which they are used. For their novel skin-interfaced monitor, the researchers selected materials that are compatible with the sensitive and fragile skin of PICU patients. They used a soft hydrogel to interface the chest device’s electrodes with the skin surface.
The team chose a robust but soft polymeric material to encapsulate the device, and demonstrated the mechanical stability of this elastomer over 70 days of shelf storage. Importantly, the researchers also autoclaved the encapsulant to establish its compatibility with the steam sterilization technique used ubiquitously in clinics. They were able to improve adhesion between the hydrogel and encapsulant materials by adding a surfactant called Silwet L-77 to the latter. The addition of just 0.2 wt% Silwet increased the peel force required to separate the two materials by 52%.
Wearable patch measures central blood pressure
Wearable patch measures central blood pressure
The researchers were able to use their device to study each of the 23 patients involved in the study, many of whom had respiratory failure, liver failure or airway abnormalities. Furthermore, the device was able to measure haemodynamic changes in response to administration of lorazepam, methadone, hydromorphone and dexamethasone, four common drugs given to intensive care patients. This points to the utility of such a monitor in guiding clinical drug management.
Looking ahead, the team hopes that these wireless smart devices could be employed outside the ICU, especially in outpatient ambulatory and in-home settings. Interfacing the device with a tablet could provide clinicians with continuous critical blood-pressure data remotely. Finally, the researchers underscore the need to expand clinical investigations and examine in detail the causes of interpatient variability in measurements.
